In these situations a caregiver or other family member is often required to sign an agreement to pay for the services before the person with special needs can. View up to date information on how Illinois is handling the Coronavirus Disease 2019 COVID-19 from the State of Illinois.
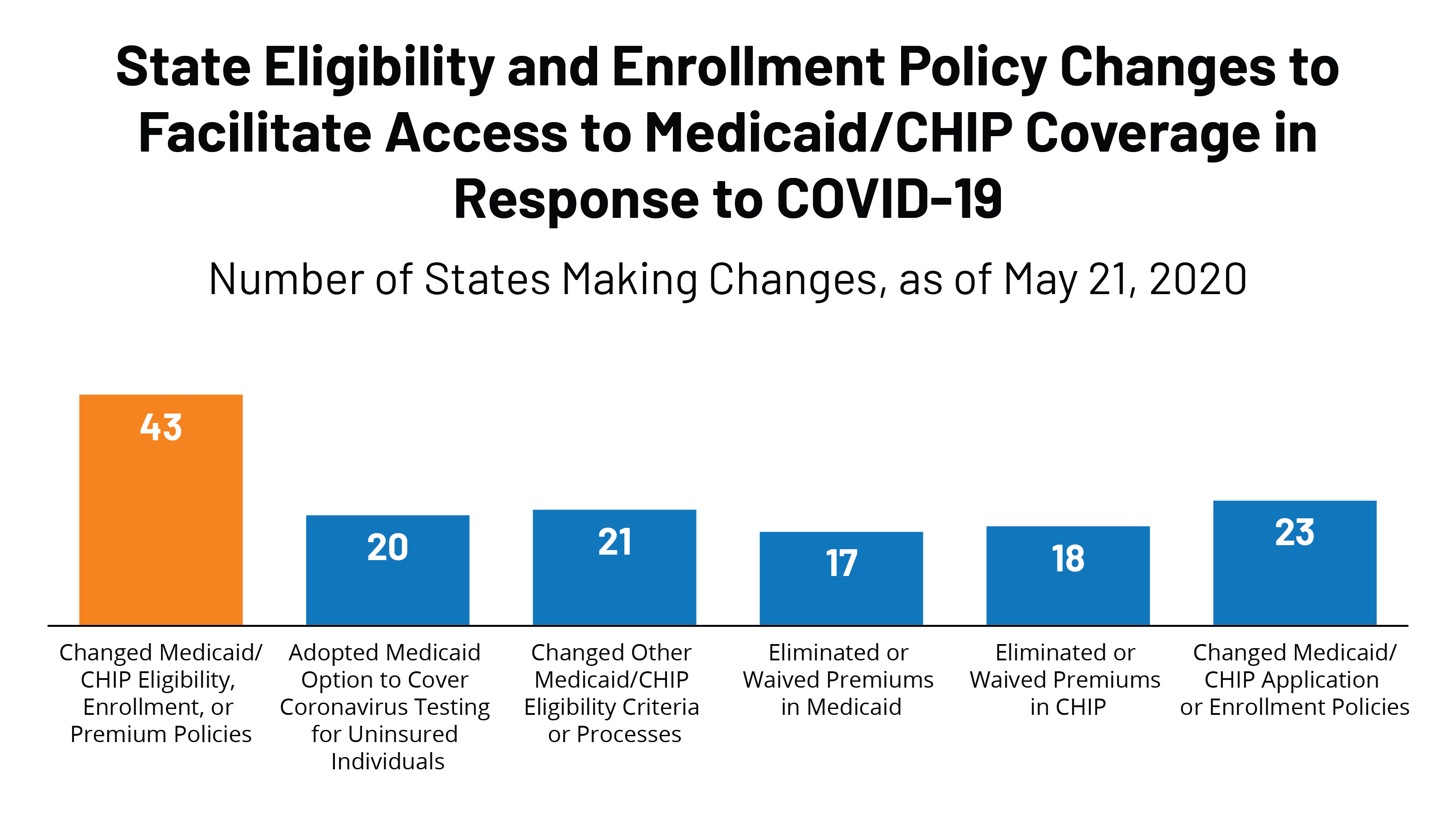 State Actions To Facilitate Access To Medicaid And Chip Coverage In Response To Covid 19 Kff
State Actions To Facilitate Access To Medicaid And Chip Coverage In Response To Covid 19 Kff
Prior approval might not be necessary if.
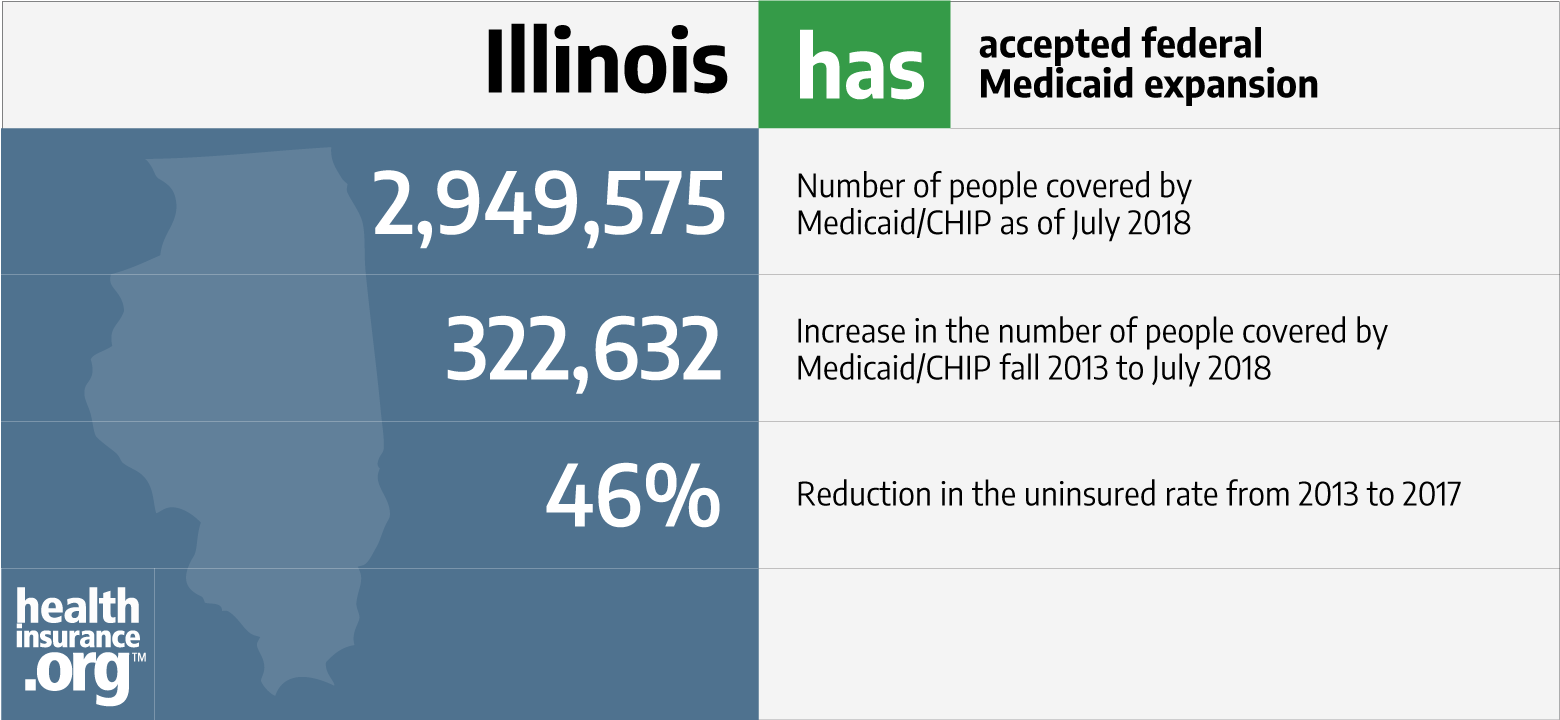
Illinois medicaid out of state coverage. Reflects Medicaid state plan coverage of the eligibility group for parents and other caretaker relatives. Links to translated versions of this FAQ. Although most Medicaid enrollees obtain medical services within their state of residence some enrollees seek care out-of-state under certain circumstances.
Under the emergency rules Medicaid members can receive services in a wider range of facilities including in their place of residence. Your Care Coordinator will assist you andor the provider in getting the necessary information to obtain prior authorization. If you need services from an out-of-network provider you or the out of network provider should contact your Care Coordinator at 1-855-580-1689 TTY.
711 Monday - Sunday 8 am. The Illinois Medicaid program covers prescription drugs as well as some over-the-counter OTC products made by manufacturers that have a signed rebate agreement with the federal Centers for Medicare and Medicaid Services CMS. Similarly Medicaid coverage may kick in if you receive treatment in an out-of-state facility that borders yours and in which residents of your state routinely seek care.
Should a beneficiary need to be admitted to a hospital in another state or if he must receive essential regular psychiatric care or medications from an out-of-state provider the home state will not pay for the services through Medicaid. Again you must make sure Medicaid will cover such care before pursuing it or you risk getting stuck with the associated bills. A medical emergency.
Seniors can sign up for one of our affordable prescription drug programs. If you arent sure if your Medicaid coverage has been approved yet or if it is still active you can check Manage My Case or call the states Automated Voice Recognition System AVRS at 1-855-828-4995 with your Recipient Identification Number RIN. Telehealth EO FAQs Medicaid Virtual Healthcare Expansion Emergency Rule FAQs.
Prescription drugs Prior approval is required for many drugs. Medicaid will cover up to 4 prescriptions a month. The Illinois Pre-Existing Condition Insurance Plan IPXP is a transitional insurance program for uninsured Illinois residents.
For a couple this threshold is 1328 per month. Current Medicaid regulations describe four situations in which states must provide out-of-state coverage. Providers should submit claims to the HRSA program for reimbursement for COVID-19 treatment for all uninsured Illinois residents who are not eligible for Medicaid the Childrens Health Insurance Program CHIP or emergency medical coverage for non-citizens due to income.
The State of Illinois Healthcare Portal a one-stop source for your healthcare needs. If you are a Medicaid customer or are uninsured and you have been asked to pay out of pocket for a COVID test or vaccine please click here and call for assistance. The Illinois Insurance Code prohibits health insurance issuers from charging higher out-of-pocket expenses to an enrollee who sees an out-of-network provider at an in-network facility if there are no in-network providers available.
National citizen permanent resident or legal alien in need of health careinsurance assistance whose financial situation would be characterized as low income or very low income. Are you a senior whos not eligible for Medicaid due to your immigration status. Medicaid Payment Policy for Out-of-State Hospital Services.
In states that use dollar amounts based on household size rather than percentages of the FPL to. Medicaid in Illinois may cover 100 percent of your healthcare costs if your individual income is less than 981 per month. However if you willfully choose a non-network provider when an in-network provider is readily available you might be subject to higher out-of-pocket expenses.
The prior approval hotline is 1-800-252-8942. The federal health reform law Patient Protection and Affordable Care Act the Affordable Care Act establishes a federally-funded temporary high risk pool to provide affordable health insurance coverage to people who have been denied insurance because of pre-existing. On Thursday March 19th Governor Pritzker issued Executive Order 2020-09 to expand telehealth services.
The state did not vote to expand coverage to include all low-income adults although the state may offer coverage to some adults with limitations and an enrollment cap. Medicaid Office Location Illinois Department of Healthcare and Family Services 201 South Grand Avenue East Springfield IL 62763. Following are links to health information and services provided by DHS and other State Agencies.
Knowing what services are covered by Medicaid and what does Medicaid not cover in Illinois is beneficial for enrollees. However the state may expand coverage to include additional claimants and medical services. In addition you have to.
Learn about Coverage. To be eligible for Illinois Medicaid you must be a resident of the state of Illinois a US. Parents and caretaker relatives with income over the income standard for coverage under this group may be eligible for coverage in the adult group in states that have expanded to cover the adult group.
We suggest contacting the Medicaid office to find out specifically what coverage is provided as it can be different in each state. Approval of a complete application for emergency medical coverage through ABEIllinoisgov is required prior to reimbursement. Women can find information on free breast and.
If you have more than 4 prescriptions you will need prior approval. Prior to receiving the services. Some prescription drugs and OTC products require prior approval from HFS before reimbursement.
In any case your income has to be less than the income limits set by the law in Illinois. To qualify for Medicaid your MAGI must be less than 150 to 196 of the FPL for children depending on age 300 for uninsured children196 for pregnant women and 17 for parentscaretakers. Medicaid must cover certain health care services according to federal mandates.
Parents can sign up their children for the states affordable health insurance programs.



